Healthcare has found itself tested in recent months. The pandemic has placed an unprecedented strain on hospitals and clinics, from an initial shortage of testing and medical supplies, to accessibility issues among rural and underserved populations, to non-Covid patients prevented from receiving treatments as entire wards are repurposed and hospitals still sealed off.
The virus has exposed fault lines in healthcare delivery that will have lasting side effects on patients and providers – 2020 may well be remembered as the time when medical interactions shifted comprehensively to digital and distributed delivery, and care systems decentralised once again.
Built For Uniformity and Volume
Large hospitals are complex structures, housing a vast range of services and units, that have developed in a patchwork manner over decades. They were able to function optimally as long as care was provided in the manner of Ford’s production line: high volume with low variability. This one-size-fits-all approach was, until recently, the norm – from care delivery to drug discovery.
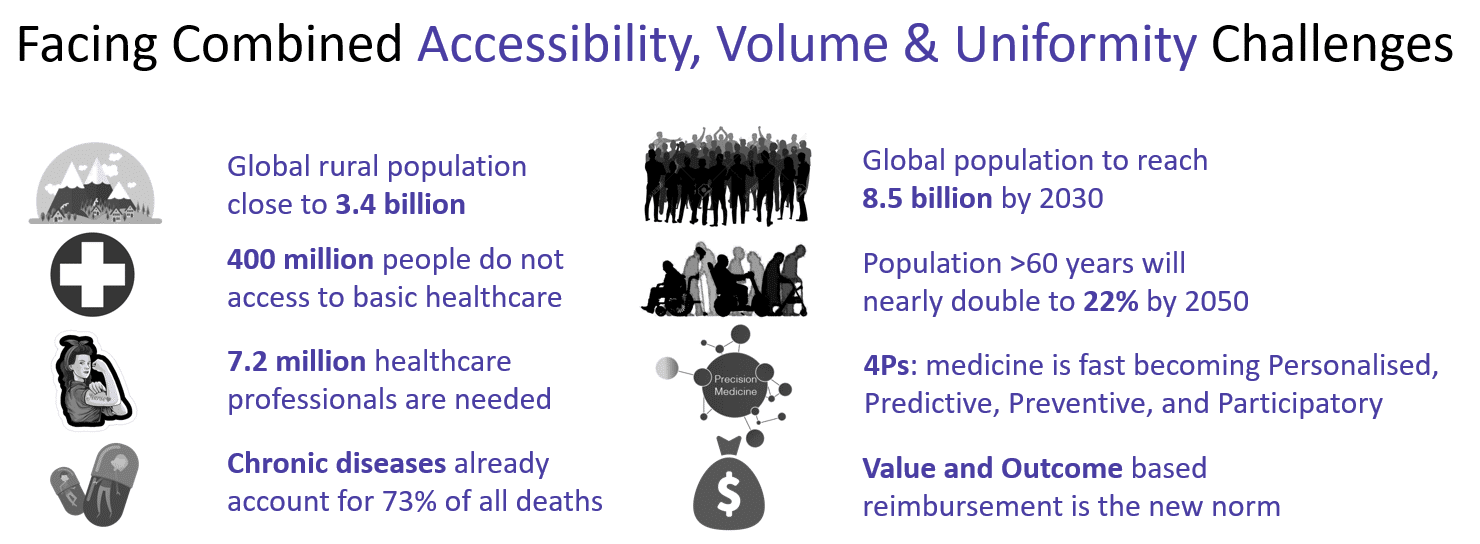
We are at an inflexion point in healthcare delivery. We have a situation where the industry is expected to deliver 21st century care – personalised, adaptive and continuous – through a rigid and localised infrastructure. The disconnect is exacerbated by a growing and ageing population, the rising prevalence of chronic diseases, unequal access to infrastructure and technological advancements, evolving payment models and higher labour costs amidst workforce shortages.
The industry as a whole, and most governments, are facing this unprecedented challenge and are actively supporting innovations that augment the capacity of existing infrastructures, all while gradually enabling decentralisation of care. This is where industry winners are emerging.
We believe that large hospitals will evolve from settings where patients often stay longer than required or frequently return to deal with chronic conditions, to centres adapted to customised treatments for complex cases, often requiring a multi-specialist approach.
It is a known fact that speed and quality of patients’ physical and mental recovery correlate with their mobility, connectivity, independence and closeness to home. As a result, patients are being moved faster out of acute care into specialist centres or into their community where they should continue to receive support.
Substantial growth opportunities lie in improving care delivery inside the hospital and providing better intervention beyond its walls.
Sometimes, solutions already exist and are hiding in plain sight. For all the advancements in connected health, the reality is that even if people are encouraged to live more healthily, monitor their biodata and access telemedicine, most medical care will still be delivered by hospitals, GPs and community nurses. As an example, considerable value can be unlocked by enhancing their workflows and delivering outstanding on-site or remote experiences.
Sometimes, solutions don’t exist and have to be invented before being integrated into care delivery systems. Think about cell and gene therapies, a new breed of treatments for diseases that have often eluded us. Today they simply cannot be delivered reliably, on time and at scale without a complete rethink of manufacturing processes and logistics.
Personalised and Decentralized Care Delivery
We invest in daring founders who often believe that the future is about fitting healthcare to the patient, not the other way around. When it comes to care delivery, I would group some of these businesses in three categories:
Technologies enabling specialist care – These are full-stack providers with a dedicated focus on certain conditions or specific domains. They go deep, vertical and provide expert end-to-end solutions to specific subpopulations of patients. These super-specialised companies can take on risk and be assertive in deploying their products.
- Congenica is the world’s leading solution for rapid genomic data analysis and clinical interpretation. It specialises in the diagnostic of genetic conditions and has become the backbone of genomic programmes across the world, starting in the UK with the 100,000 Genomes initiative.
- Igenomix has pioneered reproductive genetics and works to make a world in which infertility is no longer an impossible barrier. They have helped thousands of couples conceive by providing robust and efficient solutions at the preconception, preimplantation and prenatal phases of their reproductive journeys.
Technologies enabling adaptative pathways – Then there are horizontal platforms that create the connective tissue between patients and providers across different care settings. The goal here is to drive efficiency in communications and care coordination.
- Lumeon is the leader in care pathway orchestration, blending together advanced care process models with patient and care team engagement to ensure best practice care delivery at substantial scale. It optimises each individual patient journey – and their medical and financial outcomes – for some of the world’s largest medical insurance and healthcare groups.
- Quibim is a new addition to the Amadeus family. It discovers and validates ultra-high accuracy and quantitative imaging biomarkers and it has one of the richest catalogues of biomarkers and non-invasive detection methodologies in the world. Quibim is a reference radiomics platform for whole-body solutions and in March it also became the official European platform for high-throughput screening of COVID-19 cases.
- Doctify is a British leader in telemedicine and care quality ratings for secondary care. They work with some of the largest healthcare groups and support patients through their journey by removing information asymmetry, inefficiency, and lack of transparency.
Technologies enabling personalised logistics – Finally, there is the ‘last mile’ of care delivery. These are companies automating, leveraging AI and the latest in instrumentation and medtech to offer new standards of care and bring the solution to the patient.
- OriBiotech is the future of cell and gene therapy manufacturing. Each patient’s personalised treatment requires a unique manufacturing process. Ori is developing patient-specific, stand-alone manufacturing units that automate and standardise the entire vein-to-vein process, allowing pharmas to bring their life-saving therapies from bench to bedside in a timely and economically viable way.
- Natrox is the gold standard for the healing of chronic wounds. It’s a fully portable and discreet device that restores mobility and independence to patients. It heals the worst of wounds systematically and at an unprecedented rate – the holy grail in wound care. It is a poster technology when it comes to continuous care being transferred from acute back to homes.
- Organox has already helped transplant hundreds of livers all over the world. Its technology is fully automated, easy-to-use and can preserve the donor organ in a functional and optimal state for up to 24 hours – 3 times longer than other methods. It is transforming logistics as organs can be delivered over thousands of miles and need not be transplanted in the middle of the night anymore, materially improving outcomes.
Healthcare As A Service
As with any industry, a large and delighted user base drives rapid growth. Over and above clinical outcome or cost-efficiency, what these selected companies have in common is that they also nail user experience. You will struggle to achieve mass adoption if you limit yourself to key opinion leaders’ endorsements or clinical evidence. These are certainly essential milestones, but they are only the first step.
Users must be front and centre for a product to take off – and they often are not the patients. Think about augmenting existing infrastructure and the workflow of nurses for instance; if they are your users, obsess about making their lives simpler. Focus on those who, day after day, run our healthcare services, often doing the impossible to keep us all safe and healthy. Help them and they will become lifelong ambassadors.

